Chronic pain is a condition where people experience pain that lasts beyond the usual recovery period, often continuing for longer than three to six months. Unlike acute pain, which is a natural signal that something is wrong in the body, chronic pain persists even after the cause, such as injury or illness, has been treated.
According to the Mayo Clinic, people with chronic pain can experience discomfort in areas like the spinal cord, back, or joints. This condition is a major challenge for healthcare providers, as it affects patients with chronic pain physically, emotionally, and socially, often interfering with daily life.
1. Introduction to Chronic Pain
Chronic pain is not just a prolonged sensation; it involves changes in how the brain and spinal cord process pain signals. Usually, pain serves as a signal that tells the body something is wrong, but in people with chronic pain, this signal keeps firing long after the initial cause has been treated.
Many experience what is called chronic primary pain, where the pain exists beyond any identifiable injury or illness. High-impact chronic pain affects one’s ability to work or carry out daily activities, with many requiring assistance from health care providers to manage their condition.
2. Causes of Chronic Pain
There are many potential causes of chronic pain, ranging from past injuries and surgery to chronic conditions like arthritis or fibromyalgia. Chronic pain can also develop without a clear cause, often referred to as chronic pain syndrome.
Cancer pain, chronic low back pain, and chronic visceral pain are among the most common types that affect individuals for years. According to the International Association for the Study of Pain, chronic pain may be associated with changes in the nervous system that occur over time, leading to persistent pain signals.
This is especially evident in people who suffer from pain after surgery or treatment for pain associated with conditions like cancer.
2.1 Chronic Pain and Medical Conditions
Many chronic illnesses, such as cancer, arthritis, and diabetes, can lead to chronic pain. For instance, chronic low back pain is commonly seen in adults who live with injuries to their spine or spinal cord.
Patients with chronic pain caused by illness often face additional challenges, as the pain can limit their ability to engage in daily activities or social interactions. People with chronic pain often require comprehensive management of chronic pain through multidisciplinary approaches, including both physical and psychological therapies.
Cognitive-behavioral therapy has shown promise in helping people reframe their relationship with pain.
2.2 Psychological and Emotional Causes
Pain is more than just a physical sensation, it’s also tied to feelings and emotions. People experiencing chronic pain often develop conditions such as anxiety or depression, which can exacerbate their pain.
According to the American College of Pain Medicine, patients with chronic pain benefit from treatments that address both the physical and emotional aspects of pain. Approaches like tai chi, which combines physical movement and mindfulness, help individuals cope with pain by reducing stress and promoting relaxation.
Additionally, cognitive-behavioral therapy helps patients modify their thought patterns to cope with their pain more effectively.
3. Symptoms of Chronic Pain
Symptoms of chronic pain vary widely but can include persistent aches, sharp feelings, burning, or stiffness. Many people find it difficult to sleep or carry out daily tasks due to their pain, which can last for weeks or even years.
Pain can occur in various forms, such as chronic visceral pain affecting internal organs or cancer pain resulting from ongoing treatments. People with chronic pain often need support to manage these symptoms, relying on programs at specialized clinics or home care.
3.1 Types of Chronic Pain
Chronic pain comes in different types. Nociceptive pain, for instance, is caused by tissue damage and is common in conditions like arthritis. On the other hand, neuropathic pain stems from nerve damage, which can occur after an injury to the spinal cord.
Identifying the type of pain is crucial for effective treatment. Healthcare providers usually conduct evaluations to determine whether a person is experiencing chronic primary pain, which often requires different treatments than secondary chronic pain caused by illness.
4. Diagnosis and Evaluation of Chronic Pain
Diagnosing chronic pain involves a thorough evaluation by a healthcare provider. Physicians look for the problem that may have triggered the syndrome and assess whether the pain is a symptom of a broader issue.
Diagnostic tests like MRI and CT scans help find the root cause. Systematic review and meta-analyses of research help determine best practices for diagnosing and managing chronic pain. In cases where pain persists longer than expected, the diagnosis may shift toward chronic pain syndrome.
Many academic sites and association for the study of pain advocate for using a comprehensive approach, combining both medical and psychological assessments.
4.1 Chronic Pain in Specialized Populations
People experiencing chronic pain may fall into specific groups, such as older adults, women, or those recovering from surgery. For instance, pain after a procedure may become chronic if not properly managed. Prevalence of chronic pain tends to increase with age, and certain conditions disproportionately affect women.
Chronic pain among older adults is often misdiagnosed, leading to inadequate treatment. Research archived from the original studies published by the Journal of Pain highlights the need for targeted interventions for these populations.
5. Management and Treatment of Chronic Pain
Treating chronic pain requires a program that addresses both the physical and emotional components of the condition. Pain treatment options range from medication, physical therapy, to alternative treatments like tai chi and cognitive-behavioral therapy.
It's essential to involve healthcare providers to manage high-impact chronic pain effectively. For many, pain medicine is part of the treatment plan, but it must be used carefully due to the risks of long-term use.
5.1 Medical Treatments
Medications, including pain medicine like NSAIDs and opioids, are common in chronic pain treatment. However, opioids must be used cautiously, especially for those with chronic primary pain where the cause of pain is not clearly identifiable.
Patients and healthcare providers need to balance the benefits of pain relief with the risks of dependence and side effects. Alternative therapies like tai chi and cognitive-behavioral therapy are increasingly recommended by the International Association for the Study of Pain.
5.2 Physical and Alternative Therapies
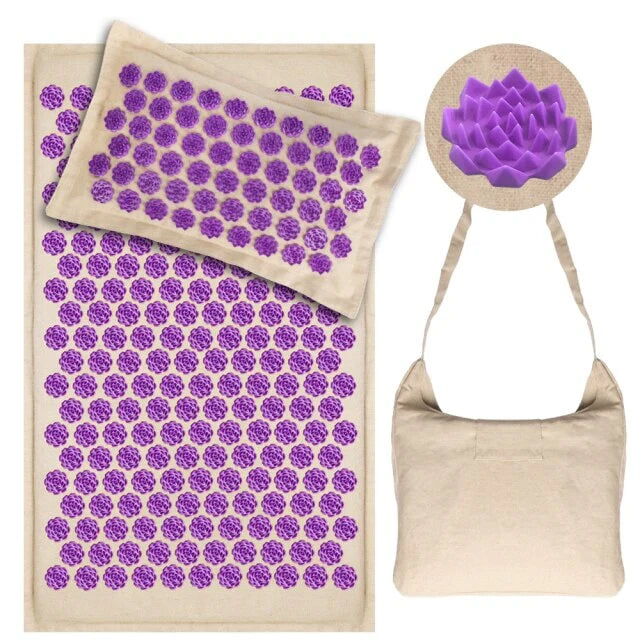
Physical therapy is an integral part of managing chronic pain, as it helps restore mobility and function. Complementary treatments like acupuncture, tai chi, and cognitive-behavioral therapy are also beneficial.
These therapies focus on improving the body's natural healing abilities and helping patients cope with pain. A systematic review and meta-analysis of various therapies suggests that these non-invasive approaches can significantly improve the quality of life for those with chronic pain.
6. Lifestyle Changes and Coping Strategies
Lifestyle changes are essential in managing chronic pain over the long term. Regular exercise, maintaining a healthy diet, and ensuring proper sleep hygiene can help mitigate the effects of chronic pain.
People can benefit from integrating relaxation techniques, such as tai chi, and working with their health care provider to develop an individualized plan. These practices help patients with chronic pain reduce stress, which is often a contributing factor in the persistence of pain.
6.1 Mind-Body Approaches
Mind-body techniques like tai chi and cognitive-behavioral therapy provide significant relief for people experiencing chronic pain. These methods help patients reframe how they experience pain, focusing on positive coping mechanisms.
Regular practice of such techniques has been shown to reduce the intensity of chronic pain and improve overall well-being, as supported by studies archived from the original Journal of Pain.
6.2 Support Networks and Communities
Support groups and communities, both online and in-person, can be a lifeline for people with chronic pain.
Organizations like the American College of Pain Medicine and the Association for the Study of Pain offer resources and programs to help patients and their families. These communities provide a space to share experiences, find new treatment options, and receive emotional support.
7. New Frontiers in Chronic Pain Research
Recent advances in chronic pain research are offering new hope to patients with chronic pain. Studies are focusing on innovative treatments like gene therapy, spinal cord stimulation, and advanced medications that target specific pain pathways.
Research conducted by the American College of Pain Medicine suggests that these new approaches could transform the way people manage high-impact chronic pain.
The Journal of Pain continues to publish emerging studies on the management of chronic pain, providing healthcare providers with up-to-date treatment options.
8. Conclusion: Living with Chronic Pain
Living with chronic pain is undoubtedly challenging, but it is possible to maintain a fulfilling life with the right strategies. Managing chronic pain requires a comprehensive approach that includes medical treatment, lifestyle changes, and emotional support.
By working closely with healthcare providers and utilizing both traditional and alternative therapies, people can learn to cope with their pain and improve their quality of life.
Frequently asked questions
1. What is chronic pain and how is it different from acute pain?
Chronic pain is pain that lasts for more than 3 to 6 months, even after the initial injury or illness has healed. It differs from acute pain, which typically goes away once the body heals. Chronic pain affects the brain and nervous system, continuing to send pain signals long after the cause is resolved.
In the United States, millions of people suffer from high-impact chronic pain, which limits their ability to work or carry out daily activities. Our mission is to help people understand chronic pain and find better ways to manage it.
2. What causes chronic pain?
Chronic pain can happen for many reasons, including injuries, surgeries, or conditions like arthritis. Sometimes the pain continues even when there’s no visible cause, a condition known as high-impact chronic pain.
Factors such as how our brain processes pain signals, nerve damage, and muscle tension can all contribute. In the United States, millions of people live with chronic low back pain, cancer pain, and other pain syndromes.
Understanding the root causes is key to finding better treatment solutions, which is the mission of many pain centers across the country.
3. What are the symptoms of chronic pain?
Chronic pain symptoms can include persistent aches, sharp or burning sensations, and muscle stiffness. These symptoms often vary in intensity from day to day.
Chronic pain can affect both physical and emotional well-being, making it hard to carry out everyday tasks. Many people with chronic pain feel fatigued and struggle with anxiety or depression.
Our understanding of how the brain processes pain helps provide better treatment options, such as cognitive behavioral therapy, which can help people manage the emotional aspects of chronic pain.
4. How is chronic pain diagnosed?
To diagnose chronic pain, healthcare providers make a thorough evaluation of the patient’s medical history, symptoms, and pain patterns. Tests such as MRI scans may be used to rule out other causes.
Diagnosis can also include an assessment of how the pain affects daily activities, which is crucial in identifying high-impact chronic pain. Sometimes, doctors will refer patients to a pain center for further evaluation and treatment.
Our goal is to provide better diagnostic tools and resources to help patients understand their condition.
5. What are the treatment options for chronic pain?
Treatment options for chronic pain include medications, cognitive behavioral therapy, physical therapy, and alternative therapies like acupuncture or yoga. In severe cases, nerve blocks or spinal cord stimulation may be recommended.
Chronic pain treatment aims to reduce pain levels and improve quality of life. Across the United States, healthcare providers work closely with patients to develop individualized treatment plans at specialized pain centers.
Effective treatments can help the pain go away or at least make it more manageable over time.
6. Can lifestyle changes help with chronic pain?
Yes, lifestyle changes can greatly improve how people cope with chronic pain. Regular exercise, a healthy diet, and proper sleep can make a big difference. Activities like tai chi and yoga, which focus on movement and relaxation, can help relieve muscle tension and reduce stress.
Cognitive behavioral therapy is another effective tool for managing pain and associated mental health issues. Chronic pain may not always goes away, but these changes can help people feel better and more in control.
7. How does chronic pain affect mental health?
Chronic pain can significantly affect mental health, often leading to anxiety and depression. This emotional strain can make physical pain worse, creating a cycle that is hard to break.
By using cognitive behavioral therapy, people can learn to change negative thought patterns and improve how they feel both physically and mentally.
In the United States, high-impact chronic pain is a leading cause of disability, affecting millions of people’s emotional well-being. Integrating mental health support into pain management is essential to help patients live better.
8. Can chronic pain be cured or prevented?
Chronic pain cannot always be completely cured, but early treatment can help make it more manageable.
Preventing chronic pain involves maintaining a healthy lifestyle, treating injuries promptly, and managing stress. In some cases, chronic pain may go away after treatment, but for others, long-term management may be necessary.
The mission of many healthcare providers is to find better ways to prevent chronic pain, and research in the United States continues to explore new treatment options.
9. What is the role of alternative therapies like tai chi and acupuncture in managing chronic pain?
Alternative therapies such as tai chi and acupuncture are increasingly recognized as effective treatments for managing chronic pain. Tai chi focuses on gentle movements that relieve tension and improve flexibility, which can help people feel better.
Acupuncture is believed to influence how the brain processes pain signals, reducing the intensity of pain. Many pain centers across the United States include these therapies as part of their comprehensive treatment programs. They are especially useful for people who prefer non-medication approaches.
10. How can I find help for chronic pain?
If you are experiencing chronic pain, it's important to seek help from a healthcare provider who specializes in pain management. Many centers across the United States focus on the diagnosis and treatment of chronic pain.
The mission of these centers is to provide better care through treatments such as cognitive behavioral therapy, physical therapy, and medication management.
Support groups and resources are also available to help people live with chronic pain more effectively. Finding the right pain management service can make a significant difference in your quality of life.